Connect With Us
Blog
Items filtered by date: August 2020
Am I at Risk for Peripheral Artery Disease?
 Peripheral artery disease or more commonly known as PAD, is a condition that causes poor circulation to the lower limbs due to plaque buildup in the arteries. This arterial plaque buildup causes the arteries to harden and narrow, leading to reduced blood flow to the affected areas. If severe enough, blocked blood flow can cause gangrene. In severe cases, this can lead to leg amputation.Some people are at an increased risk of developing PAD. The main risk factor for developing PAD is smoking or having a history of smoking. Other risk factors include having a history of diabetes, high blood pressure, high cholesterol, ischemic heart disease, stroke, and metabolic syndrome. If you have any of these risk factors, discuss them with a podiatrist, who can monitor the health of your lower limbs and screen for PAD.
Peripheral artery disease or more commonly known as PAD, is a condition that causes poor circulation to the lower limbs due to plaque buildup in the arteries. This arterial plaque buildup causes the arteries to harden and narrow, leading to reduced blood flow to the affected areas. If severe enough, blocked blood flow can cause gangrene. In severe cases, this can lead to leg amputation.Some people are at an increased risk of developing PAD. The main risk factor for developing PAD is smoking or having a history of smoking. Other risk factors include having a history of diabetes, high blood pressure, high cholesterol, ischemic heart disease, stroke, and metabolic syndrome. If you have any of these risk factors, discuss them with a podiatrist, who can monitor the health of your lower limbs and screen for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Rouder from S.I. Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Am I at Risk for Peripheral Artery Disease?
 Peripheral artery disease or more commonly known as PAD, is a condition that causes poor circulation to the lower limbs due to plaque buildup in the arteries. This arterial plaque buildup causes the arteries to harden and narrow, leading to reduced blood flow to the affected areas. If severe enough, blocked blood flow can cause gangrene. In severe cases, this can lead to leg amputation.Some people are at an increased risk of developing PAD. The main risk factor for developing PAD is smoking or having a history of smoking. Other risk factors include having a history of diabetes, high blood pressure, high cholesterol, ischemic heart disease, stroke, and metabolic syndrome. If you have any of these risk factors, discuss them with a podiatrist, who can monitor the health of your lower limbs and screen for PAD.
Peripheral artery disease or more commonly known as PAD, is a condition that causes poor circulation to the lower limbs due to plaque buildup in the arteries. This arterial plaque buildup causes the arteries to harden and narrow, leading to reduced blood flow to the affected areas. If severe enough, blocked blood flow can cause gangrene. In severe cases, this can lead to leg amputation.Some people are at an increased risk of developing PAD. The main risk factor for developing PAD is smoking or having a history of smoking. Other risk factors include having a history of diabetes, high blood pressure, high cholesterol, ischemic heart disease, stroke, and metabolic syndrome. If you have any of these risk factors, discuss them with a podiatrist, who can monitor the health of your lower limbs and screen for PAD.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Rouder from S.I. Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Peripheral Artery DiseaseDo I Have Plantar Warts?
 Pain felt on the soles of the feet can be indicative of a condition known as plantar warts. The appearance of plantar warts can be compared to thickened, callused skin, however they often have tiny black dots in their center. Because they’re normally found on the soles of the feet, plantar warts can run the risk of being pushed inward as one walks. Some have described feeling as if a pebble is stuck in their shoe when the plantar warts are pushed inward. For a proper diagnosis and advised treatment plan for plantar warts, please seek the care of a podiatrist.
Pain felt on the soles of the feet can be indicative of a condition known as plantar warts. The appearance of plantar warts can be compared to thickened, callused skin, however they often have tiny black dots in their center. Because they’re normally found on the soles of the feet, plantar warts can run the risk of being pushed inward as one walks. Some have described feeling as if a pebble is stuck in their shoe when the plantar warts are pushed inward. For a proper diagnosis and advised treatment plan for plantar warts, please seek the care of a podiatrist.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Rouder from S.I. Podiatry. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about What Are Plantar Warts?Do I Have Plantar Warts?
 Pain felt on the soles of the feet can be indicative of a condition known as plantar warts. The appearance of plantar warts can be compared to thickened, callused skin, however they often have tiny black dots in their center. Because they’re normally found on the soles of the feet, plantar warts can run the risk of being pushed inward as one walks. Some have described feeling as if a pebble is stuck in their shoe when the plantar warts are pushed inward. For a proper diagnosis and advised treatment plan for plantar warts, please seek the care of a podiatrist.
Pain felt on the soles of the feet can be indicative of a condition known as plantar warts. The appearance of plantar warts can be compared to thickened, callused skin, however they often have tiny black dots in their center. Because they’re normally found on the soles of the feet, plantar warts can run the risk of being pushed inward as one walks. Some have described feeling as if a pebble is stuck in their shoe when the plantar warts are pushed inward. For a proper diagnosis and advised treatment plan for plantar warts, please seek the care of a podiatrist.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Rouder from S.I. Podiatry. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Preventing Cycling Injuries
 Cycling is becoming increasingly popular as a form of exercise. However, as a cyclist, you must be wary of injuries to your ankle or foot. Luckily, there are preventative measures that you can take to save yourself from the pain of an injury. One of the most common ankle injuries from cycling is Achilles tendonitis, an overuse injury of the tendon that runs from the calf muscle to the back of the foot. Training too much, or too hard too quickly, can increase your risk of Achilles tendonitis. To help prevent this injury, try to break up your cycling to allow adequate time for rest and healing. Another common problem among cyclists is foot numbness. This may be caused by ill-fitting shoes or a lot of uphill riding. To help prevent foot numbness, make sure that you are wearing properly-fitted shoes, and add more variety to your rides so that you are not always cycling uphill. For more information on how to prevent and treat cycling injuries of the feet and ankles, talk to a podiatrist today.
Cycling is becoming increasingly popular as a form of exercise. However, as a cyclist, you must be wary of injuries to your ankle or foot. Luckily, there are preventative measures that you can take to save yourself from the pain of an injury. One of the most common ankle injuries from cycling is Achilles tendonitis, an overuse injury of the tendon that runs from the calf muscle to the back of the foot. Training too much, or too hard too quickly, can increase your risk of Achilles tendonitis. To help prevent this injury, try to break up your cycling to allow adequate time for rest and healing. Another common problem among cyclists is foot numbness. This may be caused by ill-fitting shoes or a lot of uphill riding. To help prevent foot numbness, make sure that you are wearing properly-fitted shoes, and add more variety to your rides so that you are not always cycling uphill. For more information on how to prevent and treat cycling injuries of the feet and ankles, talk to a podiatrist today.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Dr. Rouder of S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Preventing Cycling Injuries
 Cycling is becoming increasingly popular as a form of exercise. However, as a cyclist, you must be wary of injuries to your ankle or foot. Luckily, there are preventative measures that you can take to save yourself from the pain of an injury. One of the most common ankle injuries from cycling is Achilles tendonitis, an overuse injury of the tendon that runs from the calf muscle to the back of the foot. Training too much, or too hard too quickly, can increase your risk of Achilles tendonitis. To help prevent this injury, try to break up your cycling to allow adequate time for rest and healing. Another common problem among cyclists is foot numbness. This may be caused by ill-fitting shoes or a lot of uphill riding. To help prevent foot numbness, make sure that you are wearing properly-fitted shoes, and add more variety to your rides so that you are not always cycling uphill. For more information on how to prevent and treat cycling injuries of the feet and ankles, talk to a podiatrist today.
Cycling is becoming increasingly popular as a form of exercise. However, as a cyclist, you must be wary of injuries to your ankle or foot. Luckily, there are preventative measures that you can take to save yourself from the pain of an injury. One of the most common ankle injuries from cycling is Achilles tendonitis, an overuse injury of the tendon that runs from the calf muscle to the back of the foot. Training too much, or too hard too quickly, can increase your risk of Achilles tendonitis. To help prevent this injury, try to break up your cycling to allow adequate time for rest and healing. Another common problem among cyclists is foot numbness. This may be caused by ill-fitting shoes or a lot of uphill riding. To help prevent foot numbness, make sure that you are wearing properly-fitted shoes, and add more variety to your rides so that you are not always cycling uphill. For more information on how to prevent and treat cycling injuries of the feet and ankles, talk to a podiatrist today.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Dr. Rouder of S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Sports Related Foot And Ankle InjuriesHow Does Morton's Neuroma Feel?
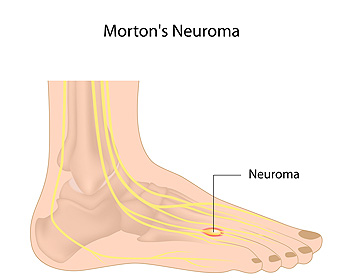 Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Rouder of S.I. Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How Does Morton's Neuroma Feel?
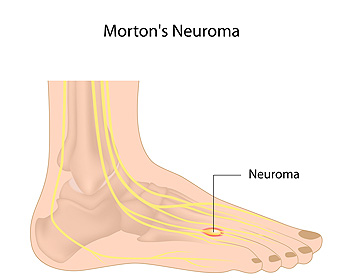 Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Rouder of S.I. Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Morton's NeuromaTypes of Bunions
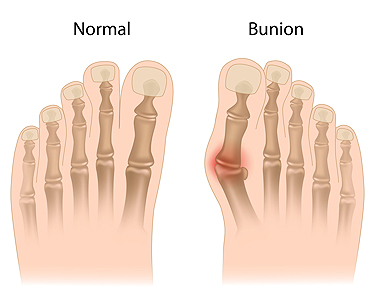 A bunion is a bony bump that forms on the joint at the base of the big toe or, occasionally, on the pinky toe. The bunion causes the affected toe to point towards the other toes, instead of pointing straight ahead. Bunions may be painful, making it difficult to walk, stand, wear your typical shoes, or do your usual daily activities. There are two main types of bunions, although many bunions can be a combination of both types. A positional bunion is caused by the joint enlarging as new bone grows. This stretches the outer covering of the joint and pushes the big toe towards the smaller ones, eventually pulling the big toe out of alignment. A structural bunion is caused by the angle between the bone of the big toe and second toe being larger than normal. This can also push the big toe towards the smaller toes. Regardless of the type of bunion you may have, it is recommended that you seek treatment from a podiatrist.
A bunion is a bony bump that forms on the joint at the base of the big toe or, occasionally, on the pinky toe. The bunion causes the affected toe to point towards the other toes, instead of pointing straight ahead. Bunions may be painful, making it difficult to walk, stand, wear your typical shoes, or do your usual daily activities. There are two main types of bunions, although many bunions can be a combination of both types. A positional bunion is caused by the joint enlarging as new bone grows. This stretches the outer covering of the joint and pushes the big toe towards the smaller ones, eventually pulling the big toe out of alignment. A structural bunion is caused by the angle between the bone of the big toe and second toe being larger than normal. This can also push the big toe towards the smaller toes. Regardless of the type of bunion you may have, it is recommended that you seek treatment from a podiatrist.
If you are suffering from bunion pain, contact Dr. Rouder of S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Types of Bunions
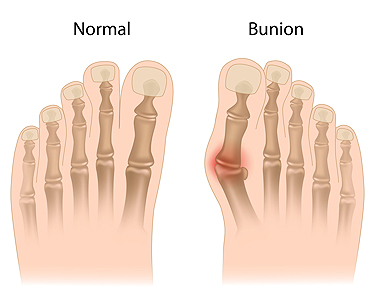 A bunion is a bony bump that forms on the joint at the base of the big toe or, occasionally, on the pinky toe. The bunion causes the affected toe to point towards the other toes, instead of pointing straight ahead. Bunions may be painful, making it difficult to walk, stand, wear your typical shoes, or do your usual daily activities. There are two main types of bunions, although many bunions can be a combination of both types. A positional bunion is caused by the joint enlarging as new bone grows. This stretches the outer covering of the joint and pushes the big toe towards the smaller ones, eventually pulling the big toe out of alignment. A structural bunion is caused by the angle between the bone of the big toe and second toe being larger than normal. This can also push the big toe towards the smaller toes. Regardless of the type of bunion you may have, it is recommended that you seek treatment from a podiatrist.
A bunion is a bony bump that forms on the joint at the base of the big toe or, occasionally, on the pinky toe. The bunion causes the affected toe to point towards the other toes, instead of pointing straight ahead. Bunions may be painful, making it difficult to walk, stand, wear your typical shoes, or do your usual daily activities. There are two main types of bunions, although many bunions can be a combination of both types. A positional bunion is caused by the joint enlarging as new bone grows. This stretches the outer covering of the joint and pushes the big toe towards the smaller ones, eventually pulling the big toe out of alignment. A structural bunion is caused by the angle between the bone of the big toe and second toe being larger than normal. This can also push the big toe towards the smaller toes. Regardless of the type of bunion you may have, it is recommended that you seek treatment from a podiatrist.
If you are suffering from bunion pain, contact Dr. Rouder of S.I. Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Staten Island, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Bunions